Bladder cancer, while not the most common form of cancer, often goes unnoticed due to a lack of public awareness. This can lead to delayed diagnosis and hinder treatment success. This blog aims to empower you with knowledge about bladder cancer, including its signs and symptoms, the importance of early detection, and various treatment options available at Ayushman Hospital & Health Services.
Understanding Bladder Cancer
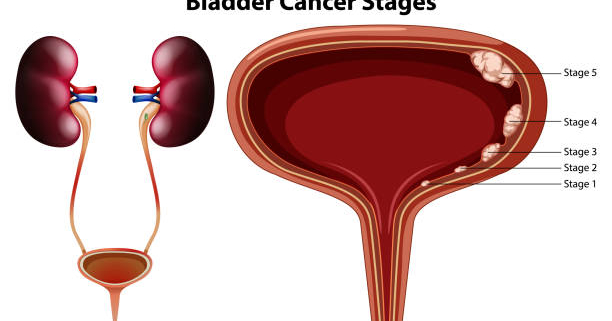
Bladder cancer begins in the cells that line the bladder, the organ that holds urine. Transitional cell carcinoma (TCC), also known as urothelial carcinoma, is the most prevalent type. TCC can be non-invasive, confined to the inner bladder layer, or invasive, spreading deeper into the bladder wall. Other types that are less frequently seen include squamous cell carcinoma and adenocarcinoma.
Warning Signs and Symptoms
Bladder cancer often presents with several telltale signs, although it’s important to remember that these can also indicate other conditions. Here’s what to watch out for:
- Blood in the Urine (Hematuria): This is a common symptom, with urine appearing pink, red, or cola-colored. While hematuria can have various causes, including infections or kidney stones, prompt investigation is crucial, especially if it recurs.
- Urinary Changes: You may experience increased urination frequency, urgency to urinate, or difficulty passing urine despite feeling the need. These can mimic a urinary tract infection (UTI) but persist despite treatment.
- Painful Urination: Burning or discomfort during urination can be a sign of bladder cancer, UTIs, or other bladder conditions. Seek medical evaluation if it persists.
- Pelvic or Lower Back Pain: As the cancer progresses, discomfort or pain may develop in the pelvic region or lower back, particularly if the cancer spreads to nearby tissues or organs.
- Weight Loss and Fatigue: Advanced bladder cancer can lead to unintentional weight loss and fatigue, often indicating a more developed stage where the cancer may have spread.
- Bone Pain: If the tumor spreads (metastasizes) to bones, pain can occur, particularly in the pelvis, spine, or long bones.
Early Detection Saves Lives
Early detection is paramount for successful bladder cancer treatment for several reasons:
- More Treatment Options: Early-stage cancer is usually confined to the inner bladder lining, allowing for less invasive procedures like cystoscopy with tumor removal or transurethral resection of bladder tumor (TURBT). These offer high success rates and positive long-term outcomes.
- Improved Prognosis: Early diagnosis significantly increases the chances of a complete cure. When detected and treated early, the likelihood of successful treatment and long-term survival is much higher. Conversely, delayed diagnosis allows the cancer to progress, making treatment more challenging and reducing the probability of a favorable outcome.
- Preserving Bladder Function: Early intervention can often preserve bladder function. In advanced stages, removing the entire bladder (cystectomy) might be necessary, significantly impacting quality of life.
- Enhanced Quality of Life: Early detection not only improves the chances of successful treatment but also allows individuals to maintain a better quality of life throughout their treatment journey. By addressing the tumor in its early stages, individuals may experience fewer symptoms and have a shorter recovery time, enabling them to resume normal activities quicker.
Treatment Options
Ayushman Hospital & Health Services offers a comprehensive range of bladder cancer treatment options tailored to individual needs, considering factors like cancer stage and grade, overall health, and patient preferences. Here’s an overview of the available treatments:
- Surgery:
- Transurethral Resection of Bladder Tumor (TURBT): This minimally invasive procedure is the most common for early-stage bladder cancer. A thin, lighted instrument is inserted through the urethra to reach the bladder, where the surgeon uses an electrical current to remove the tumor. TURBT can also be used for diagnosis.
- Radical Cystectomy: This surgical procedure entails removing the entire bladder, along with adjacent lymph nodes and nearby organs. It’s typically recommended for invasive bladder cancer that has spread beyond the inner lining. After surgery, a urinary diversion is created, such as an ileal conduit (using a part of the small intestine) or a neobladder (a pouch from a nearby intestine) to allow urine to leave the body.
- Chemotherapy: Chemotherapy medications can be used before or after surgery (neoadjuvant or adjuvant chemotherapy) for muscle-invasive bladder cancer (MIBC) to shrink tumors, reduce recurrence risk, or treat advanced cancer. In some cases, it may be the primary treatment for individuals who cannot undergo surgery.
- Immunotherapy: Immunotherapy drugs are increasingly used for advanced or metastatic bladder cancer that has not responded well to other treatments. These medications work by stimulating the body’s immune system to target and destroy cancer cells.
- Radiation Therapy: Radiation therapy employs high-energy X-rays or other types of radiation to eliminate cancer cells or reduce tumor size. There are two main types used for bladder cancer:
- External Beam Radiation Therapy: This type is the most frequently encountered. A large machine outside the body directs beams of radiation precisely at the tumor and surrounding tissues.
- Internal Beam Radiation Therapy (Brachytherapy): In some cases, a radioactive implant may be placed directly into the bladder for a short period. This approach delivers a concentrated dose of radiation to the tumor while minimizing exposure to healthy tissues.
Conclusion
Bladder cancer is a treatable condition, especially when detected early. By understanding the signs and symptoms, and taking a proactive approach to your health, you can significantly improve your chances of a successful outcome. If you experience any concerning symptoms, don’t hesitate to seek medical advice at Ayushman Hospital & Health Services. Timely diagnosis and treatment are essential for achieving the best results. Remember, understanding empowers you to manage your health proactively. Share this information with your loved ones and encourage them to prioritize regular checkups and screenings.