Arthritis is a widespread condition affecting millions of people globally, causing significant pain, stiffness, and inflammation in the joints. While there’s no cure, various treatment options and lifestyle modifications can effectively manage symptoms and improve quality of life. This guide delves into the different types of arthritis, their causes, diagnosis, treatment strategies, and helpful tips for living well with the condition.
What is Arthritis?
Arthritis refers to a group of over 100 conditions that damage your joints, the areas where two bones meet. The natural wear and tear of daily activities, injuries, or underlying health issues can contribute to arthritis development. The condition primarily affects the hands, wrists, knees, hips, feet, ankles, shoulders, and lower back.
Types of Arthritis
The most common forms of arthritis include:
- Osteoarthritis (OA): This “wear-and-tear” arthritis is the most prevalent type, typically affecting adults over 50. The cartilage cushioning your joints gradually breaks down over time, causing pain, stiffness, and reduced flexibility.
- Rheumatoid Arthritis (RA): An autoimmune disease where the immune system mistakenly attacks the joints, leading to inflammation, pain, swelling, and joint deformity. RA can affect any joint and often progresses symmetrically (affecting both sides of the body).
- Gout: This sudden and severe arthritis flare-up occurs when excess uric acid in the blood crystallizes and deposits in joints, most commonly the big toe. The pain can be excruciating.
- Ankylosing Spondylitis: Primarily affecting the spine, this inflammatory arthritis causes pain, stiffness, and fusion of the spinal joints. It often starts in the lower back and progresses upwards.
- Psoriatic Arthritis: Associated with the skin condition psoriasis, this arthritis can cause pain, swelling, and stiffness in various joints, along with characteristic changes in the fingernails and toenails.
- Juvenile Arthritis: This form of arthritis affects children and teenagers under 16. It can be challenging to diagnose as symptoms may mimic other childhood illnesses.
Symptoms and Causes of Arthritis
The most common symptoms of arthritis include:
- Joint pain, ranging from dull aches to sharp, stabbing pain.
- Swelling or inflammation around the affected joint.
- Reduced range of motion in the joint.
- Tenderness or sensitivity to touch.
- Warmth or redness around the joint.
The specific cause of arthritis varies depending on the type:
- Osteoarthritis: Primarily caused by cartilage breakdown due to aging and wear and tear.
- Rheumatoid Arthritis: An autoimmune disease with unknown triggers. Genetics and environmental factors may play a role.
- Gout: Develops due to high uric acid levels in the blood, often caused by diet, certain medications, or underlying health conditions.
- Ankylosing Spondylitis: The exact cause is unknown, but genetics are believed to be a significant factor.
- Psoriatic Arthritis: Occurs in people with psoriasis, potentially due to an overactive immune system.
- Juvenile Arthritis: The cause is unknown, but genetics and environmental factors are suspected to contribute.
Diagnosis and Tests
Diagnosing arthritis often involves a combination of a physical examination, a discussion of your medical history and symptoms, and imaging tests. During the physical exam, your healthcare provider will assess the affected joints for pain, swelling, tenderness, and range of motion.
Imaging tests may include:
- X-rays: To visualize bone abnormalities and joint damage.
- Ultrasound: To assess soft tissues like tendons and ligaments around the joint.
- Magnetic Resonance Imaging (MRI): To create detailed images of bones, soft tissues, and inflammation within the joint.
- Computed Tomography (CT) scan: To provide detailed cross-sectional images of bones and soft tissues.
Blood tests may also be conducted to check for uric acid levels (for gout) or rule out other underlying conditions.
Management and Treatment
While there’s no cure for arthritis, various treatment options can effectively manage symptoms and improve your quality of life. The specific treatment plan will depend on the type of arthritis, severity of symptoms, and your overall health. Common treatment approaches include:
- Over-the-counter (OTC) pain relievers: Medications like acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen can help reduce pain and inflammation.
- Prescription medications: Stronger pain relievers, disease-modifying antirheumatic drugs (DMARDs) for rheumatoid arthritis, or corticosteroids (powerful anti-inflammatory medications) may be prescribed by your healthcare provider.
- Physical and Occupational Therapy: Occupational therapists can help you modify daily activities to minimize joint stress and maximize your independence.
- Assistive devices: Canes, walkers, braces, or splints can provide support and stability, helping you perform daily tasks with greater ease.
- Heat and cold therapy: Applying heat (heating pads, warm baths) or cold (ice packs) to affected joints can help manage pain and inflammation.
- Weight management: Maintaining a healthy weight reduces stress on weight-bearing joints like knees and hips, potentially improving symptoms.
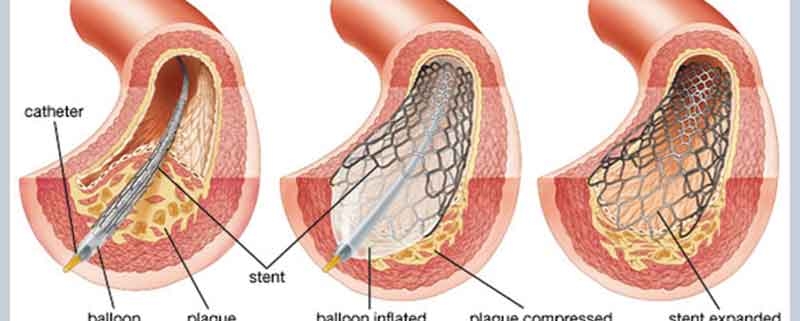
- Surgery: In instances of severe conditions where alternative treatments prove ineffective in delivering sufficient relief, surgery might be contemplated. Joint replacement surgery (arthroplasty) is a common option to replace damaged joints with artificial implants. Joint fusion surgery may also be an option for specific joints.
Prevention
While some forms of arthritis are unavoidable due to aging or genetics, certain lifestyle modifications can help reduce your risk or delay the onset of symptoms:
- Maintain a healthy weight: Excess weight puts extra stress on your joints, particularly weight-bearing ones.
- Exercise regularly: Low-impact exercises like walking, swimming, or cycling can strengthen muscles, improve flexibility, and maintain joint health.
- Eat a balanced diet: Choose a nutritious diet rich in fruits, vegetables, and whole grains to support overall health and potentially reduce inflammation.
- Protect your joints: Practice proper posture and avoid activities that put excessive stress on your joints.
- Don’t smoke: Smoking can worsen arthritis symptoms and increase the risk of developing rheumatoid arthritis.
Living With Arthritis
Arthritis is a long-term condition requiring ongoing management. Here are some tips for living well with arthritis:
- Be informed: Educate yourself about your specific type of arthritis and its management options.
- Partner with your healthcare provider: Maintain regular appointments with your doctor or rheumatologist to discuss your symptoms and treatment progress.
- Manage stress: Stress can exacerbate arthritis symptoms. Consider relaxation techniques like yoga, meditation, or deep breathing exercises.
- Join a support group: Connecting with others who understand the challenges of arthritis can provide emotional support and valuable advice.
- Stay active: Regular physical activity is crucial for maintaining joint health and reducing stiffness. Choose exercises that are gentle on your joints and modify them as needed.
- Listen to your body: Pay attention to your pain levels and adjust your activities accordingly. Don’t push yourself through severe pain.
- Prioritize sleep: Adequate sleep allows your body to heal and repair itself, which can help manage pain and inflammation.
- Maintain a positive attitude: Focus on what you can control and celebrate your achievements.
Additional Considerations
- Weather and Arthritis: Some people with arthritis experience worsened symptoms during cold or humid weather. Dress warmly in cold weather and consider using a dehumidifier at home if humidity seems to trigger your pain.
- Complementary and Alternative Therapies: Some people find relief with complementary therapies like acupuncture, massage, or fish oil supplements. However, it’s essential to discuss these options with your healthcare provider before starting them.
Conclusion
Arthritis can be a challenging condition, but with proper management and lifestyle modifications, you can take control and live a fulfilling life. Remember, early diagnosis and treatment are crucial for preventing joint damage and maintaining a good quality of life. Reach out to your healthcare provider if you experience any persistent joint pain or stiffness.
At Ayushman Hospital & Health Services, we understand the impact arthritis can have on your daily life. Our team of experienced rheumatologists, orthopedic surgeons, physiotherapists, and other healthcare professionals is dedicated to providing comprehensive care for all types of arthritis. We offer a personalized approach to treatment, focusing on pain management, improving joint function, and preventing further damage.